December 2021: The Omicron variant, first identified in South Africa, is in the process of sweeping the globe — on December 15, the UK reported the highest number of COVID cases since the pandemic began: more than 78,000 in the past 24 hours. Because the Omicron variant is much more infectious than the Delta variant, the number of cases in most countries is expected to expand rapidly. “If you have 100,000 cases today, it’s 200,000 cases [in] two days, 400,000 two days later, and then it’s 800,000 two days later,” a WHO official said. “So in a week, the actual number of cases can increase eight or tenfold.”
Medical authorities say even if the Omicron variant proves to be milder than Delta — which some early studies and anecdotal evidence from South Africa seem to suggest it might be — because of the higher reproductive or “R nought” rate, this could still overwhelm intensive-care units and hospitals, many of which are already stretched due to the previous waves of the virus, and patients who should have gone to the hospital but didn’t, and are therefore in worse shape. Some early studies appear to show that Omicron is much more prevalent in the nose and throat, and much less prevalent in the lungs, which could explain both the less serious symptoms and the higher rate of infection.

One optimistic note is that for those who have been vaccinated and boosted with Pfizer, early evidence — primarily from lab tests, rather than real-world data — is that two shots are only about 35 percent effective at preventing serious illness or death from the Omicron variant, but that the third booster brings the level of protection back up to the 90-percent range, similar to what it had against Delta (Pfizer said that research shows its COVID pill is also effective against the Omicron variant). One important aspect of the lab tests is that they only measured antibody production, but the body’s multi-level defenses consist of antibodies and also other elements, such as T cells, and focusing only on antibodies can distort the picture, some scientists say.
November 2021 update: As of November 26, the WHO said that there have been a little less than 260 million cases worldwide, and more than 5 million deaths — a number that most experts believe significantly understates the total amount of COVID-related deaths. When I looked at the data on November 28, there had been more than 600,000 new cases in the past 24 hours. In many places, vaccination rates are high — more than 85 percent of Canadians are double vaccinated, and many have also had boosters — so while cases are rising, the number of hospital admissions and deaths is not rising as quickly.

Nevertheless, some countries, including Germany, started locking down again even before the new Omicron variant was discovered and labeled a “variant of concern” by the WHO, which happened on November 26. The new variant was first isolated in South Africa, which led a number of countries to stop allowing any incoming flights from that country, even though the variant is likely already elsewhere, and experts say the only reason South Africa found it is that their detection and analysis systems are first rate. Cases have already been detected in the UK and a number of other countries.
One of the reasons the Omicron variant is seen as concerning is that it has a far greater number of mutations than other variants, and many of them appear to be similar to mutations that have allowed the Delta variant to infect people despite the fact that they are vaccinated. There is also some evidence that the Omicron variant spreads quickly, but there are still a lot of unknowns, including how severe the infections are in those who have been vaccinated. Experts say we should know more within a couple of weeks, and that Pfizer and Moderna believe they can easily create new vaccines to attack the new variant.
June 18 update: According to official estimates, more than 3.8 million people have died of COVID worldwide, out of a total of 178 million official cases, and the death rate seems to be declining as we move down the slope of the third wave (although it should be noted that the real mortality rate and case fatality rate or CFR are not easy to calculate). That’s better than the 50 million people who are estimated to have died of the 1918 flu, but still a huge number. In the US, more than 600,000 people have died — that’s more than died in the Second World War, the Vietnam War and the Korean War put together. It’s also important to note that the research shows as many as 25 percent of people who recover from COVID develop long-term symptoms, including brain changes.
As we head into summer, things are looking up, at least in North America and Europe. New York just announced they are opening up — including dining inside restaurants at full capacity — because infection and hospitalization rates are low and the number of people with at least one vaccination has passed 70 percent. There are still some restrictions (producers of a Broadway show with Bruce Springsteen won’t let anyone who got the Astra-Zeneca vaccine attend a play, for example, because it never got licensed in the US). My wife Becky and I both got our second shot of Pfizer a couple of weeks ago, so according to the research we should be at greater than 90 percent protection against hospitalization and death from COVID, and that apparently includes the so-called Delta variant — previously known as the India variant, because that’s where it is said to have originated.
Because it’s estimated to be about 50 percent more contagious than the previous virus, the Delta version is now the dominant variant in the UK, and it’s rapidly increasing in the US as well — doubling every 12 days or so. The variant also carries a much greater risk of hospitalization, and it also affects children much more often than the earlier versions, both of which are concerning. But on the brighter side, vaccination rates are surging in North America and most of Europe, so that should keep the Delta variant contained more than it would be otherwise. In much of the African continent, however, and in countries that have health-care and/or political challenges, COVID continues to rage, and only a small proportion of the population has been vaccinated even once.

How will that affect global travel as the world starts opening back up? Will countries that have remained safe due to closing their borders quickly, like Australia, be loathe to open up again? Will there be a global vaccine passport? How quickly will there be a rollout of a potential third shot booster for the Delta variant, or new variants that emerge? All questions that remain unanswered. On another bright note, scientists are using the knowledge they have gained about mRNA vaccines to work on shots that might help with dozens of other diseases, including malaria and even cancer.
April 2021 update: It’s been over a year now since COVID became a reality for most of us in North America. We came back from our vacation in Florida on March 17th or so to a changed world, and it has continued to change rapidly ever since. My 85-year-old mother got COVID in December — as did about 120 people in her retirement home — but it was a relatively mild case and she turned out to be fine after a couple of weeks in hospital. Vaccines are being rolled out (with varying degrees of success) in most countries. After a rocky start, President Joe Biden seems to have gotten things moving in the US and more than 100 million people have gotten their first shot of one of the vaccines. In Canada, supply constraints held things back, but they are rolling out now — my wife Becky and I have gotten our first shot of the Pfizer mRNA vaccine because we are caregivers for my mother, and our second shot has been pushed out several months in order to give others the chance to get a first one (Pfizer appears to be about 80 percent effective after one shot).
The US has agreed to give Canada a bunch of Astra-Zeneca doses because it hasn’t been approved in the US yet and they will expire before it does. There have also been a number of countries that have paused or held back on providing A-Z vaccine because of about 20 cases of abnormal clotting, including some deaths — despite the fact that studies show the number of cases (plus or minus 20 out of 17 million) is well below the normal incidence of fatal blood clots. Pfizer and Moderna look to be about 90 percent effective in the real world against contracting a symptomatic case of COVID, and 100 percent effective against hospitalization or death. What remains unknown is how effective the various vaccines are against the new variants, the worst of which seems to be the British one, B117, which is significantly more contagious than the original, and also more lethal, and seems to be infecting more younger people than the previous one.

In Ontario, more than 65 percent of cases are now the British variant, and the ICUs are filling up. After a decline in the early part of the year, we and others are now well into the third wave, with case numbers rising sharply and more people being hospitalized. Ontario just went into a month-long lockdown, even though Toronto, Hamilton, Peel and other regions were already in the “grey” zone, meaning they were supposed to be locked down already. As in a number of other places, Ontario in particular seems to have struggled to find a balance between locking down quickly to prevent spread (the way countries like South Korea and New Zealand have) and keeping things open to help restaurants and other small businesses, and to keep schools open as a way of helping both kids and parents. “I’m going to pause here. I’m going to lose the script, and I’m going to reflect on the recurring feeling I have of impending doom,” CDC director Rochelle Walensky said recently.
January 2021 update: It’s now been a year since a brave Chinese researcher released the genome of the COVID-19 virus, against the wishes of his government, which allowed vaccine makers to get to work on new mRNA or modified RNA vaccines even before the first case was identified in the United States. Two of those vaccines — from Moderna and Pfizer — started rolling out in November (see below), although the rollout in both the US and Canada has been slow, for a variety of reasons, one of which is the fact that both vaccines need to be kept at extremely cold temperatures and plenty of places don’t have those kinds of facilities. A new Johnson & Johnson vaccine is supposed to be available soon, and it is a traditional vaccine that uses part of the virus itself as the delivery vehicle, and therefore doesn’t need special storage requirements.
That’s the good news. The bad news (in addition to the recent riot in which armed goons stormed the US Capitol, breaching its security for the first time since the 1950s, in what seemed to be an attempt to reverse the results of the election) is that there are at least two new strains of the virus that are causing concern, one that was first identified in the UK and one first identified in South Africa. They are both believed by some researchers to be more infectious than the original strain — up to 70 percent more infectious. Epidemiologists and other researchers note that viruses like COVID always evolve over time, and sometimes rapidly — measles mutates very slowly, so shots are good for years, but the regular flu mutates quickly, so you need a different shot every year. It’s still not clear which of these COVID will be more like. There is some evidence that the current vaccines may be effective against the new variants.

More bad news: A number of countries are seeing outbreaks and uncontrolled spread as bad or worse as the original outbreak in March of 2020, either because of a lack of stringent controls, a lack of desire on the part of people to wear masks, etc. and/or cases of the newer, more infectious variants. In the UK, authorities confirmed more than 62,000 cases in just 24 hours; according to a number of observers, both Sweden and Japan are paying the price for having been too lenient with their lockdowns and other measures early on. The US, meanwhile, has been the victim of a combination of the Trump government’s incompetence and American “every man for himself” individualism: roughly 400,000 people have now died of COVID, and the country has about 25 percent of the cases worldwide, despite only having 4 percent of the world’s population. The death rate in the US is now the equivalent of six fully-loaded 747 jumbo jets crashing and killing everyone on board, every single day.
To complicate matters, many people still refuse to wear masks, either because they think it’s an infringement on their rights, or because they believe they don’t work or are actively bad for you. And on top of that, even some front-line health workers have said they don’t plan to get the vaccine — in several counties in California, more than 50 percent of the doctors and nurses and other hospital workers who were eligible for the vaccine said they weren’t planning to get it. Also, the Wall Street Journal says the actual death rate for COVID is closer to 3 million worldwide, not 2 million.
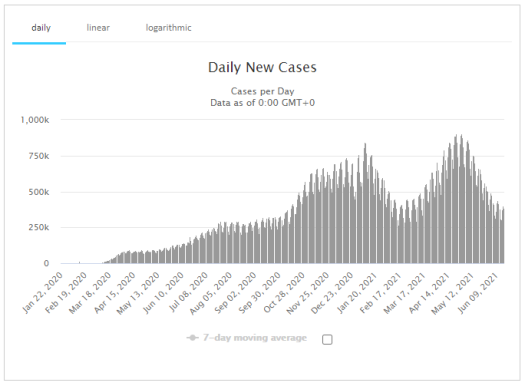
November 2020 update: The US continues to set new records for cases — 181,000 on November 13, up about 75 percent from two weeks earlier. Deaths rose by 34 percent, with 1,380 people dying on November 13 and 68,000 people hospitalized (up 41 percent). Looking at a graph of the number of new cases plotted as a seven-day moving average, it’s obvious the US is in the third wave of the pandemic. There are a total of more than 10 million people in the country that have had COVID-19. Despite the continuing climb in numbers, however, there are still those in the US who believe that COVID is “under control,” that we have to “learn to live with it” (as soon-to-be former president Donald Trump put it) and that wearing masks and other precautions are not necessary. Even in Canada there have been tensions between governments that have imposed mask rules, and those who believe that such laws are an infringement on their rights. This also happened during the 1918 flu.
As you can see from the above graph, the US is entering a third wave, much higher than the previous two. The 1918 flu followed a similar trajectory: a small initial wave, followed by a summer lull, and then a much higher wave in the fall and winter. Almost all 50 states are in what experts call an “unrestrained spread” category, with positivity rates climbing, and some are close to or at their limit in terms of ICU beds. On the upside, mortality rates seem to be advancing at a lower rate than in earlier waves — in part because doctors have gotten better at treating patients with COVID — but it’s also worth noting that deaths lag testing by about three weeks. And American Thanksgiving could be a very difficult time, with many people desperate to get together with family, combined with “pandemic fatigue,” where some people seem fed up with all of the quarantining and mask-wearing, and are either uninformed about the risks or willing to take them. Experts also say many people are dealing with mental health issues as a result of being quarantined, especially the elderly.
The graphic below comes from an interactive map designed by researchers at Georgia Tech, which displays the odds of you encountering someone with COVID, based on the number of people at an event and the testing results from counties across the US. So for example, if you are at an event with 25 or more people in much of the Midwest, there’s a better than 80 percent chance that someone at that event has COVID. And for much of the US, the odds are better than 50 percent that there will be an infected person at any event with more than about 25 people. Many countries in Europe are also going back into lockdown because their rates are climbing faster than they did during the first outbreak, and there seems to be a consensus that Sweden’s attempt to keep things open and pursue a “herd immunity” strategy is a failure.

On the upside, two companies claim that their vaccines are showing effective rates of greater than 95 percent in trials: Pfizer and Moderna also both say they expect to be able to provide millions of doses of their vaccines by the end of the year, and hopefully billions of doses by next year. Both vaccines are based on a similar approach, using mRNA in a way that causes the body to create a version of the “spike protein” that COVID uses to attach itself, which triggers the body to produce antibodies that fight off any infection. One downsize of the Pfizer version, however, is that it needs to be kept at extremely low temperatures — around -70 degrees Fahrenheit, which requires liquid nitrogen — and patients have to get two doses, three weeks apart. It’s also unknown how long the immunity provided by the vaccine lasts — some research has shown that people who get COVID are only immune for a few months.
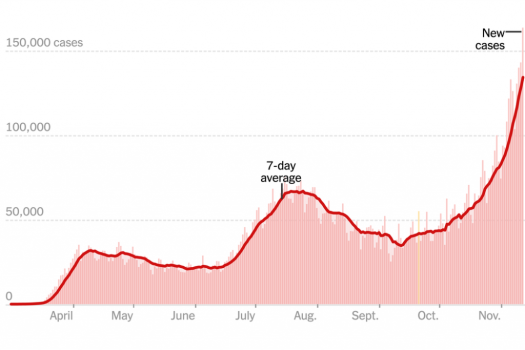
June 2020 update: The US just set a new record high for the number of daily coronavirus cases — more than 40,000 of them, which surpasses the previous record set in April. According to the CDC, as many as 20 million Americans may be infected, or 10 times the official estimates. There’s a debate over whether the upsurge in cases is a “second wave” or just an extension of the first wave, which the US failed to control properly, but regardless, cases are rising in more than 30 states. Just two months ago, they were rising in only four states, according to this virus-tracking site created by the co-founders of Instagram, which uses official case data.
Florida, Montana, Nevada, and Arizona are currently among the worst hit — a number of states are starting to close down some of the businesses they had previously allowed to re-open. Meanwhile, there are still people who refuse to wear masks, and medical officers in two states who tried to mandate mask-wearing received death threats and one resigned. Also of concern: Experts say younger people are now accounting for a disturbing number of new cases, and research shows that even those who recover from the virus could suffer long-term health effects.

Below is the text of my original post, which I wrote most of on or around March 20th after getting back from vacation in Florida, when the virus was just starting to become a serious problem. I updated the numbers in it multiple times over the next two months, but am leaving it here as part of the historical record of this crazy time.
The title of this post is a reference to the famous Gabriel García Márquez book “Love in a Time of Cholera.” I thought it was fitting was because it feels as though COVID-19 is our version of the cholera epidemic of the 1800s, or the Spanish flu of 1918 (which wasn’t Spanish at all, but probably originated in Kansas and was a form of H1N1) or the Black Death of the 1300’s. Those changed the way we lived forever, in thousands of small ways (as this piece argues that COVID-19 will), and I find myself wondering what it would have felt like if Twitter and Facebook and the Internet had been around during the Plague years. Would they have made fun of people wearing “plague masks” that made them look like giant birds? (Side note: Here’s the story of an Italian town that beat the plague, and how they did it).

I know for sure that if social media existed during the Middle Ages, they would have been full of posts that said things like “my sister is a doctor, and she says gargling with vinegar can cure the plague!” (one popular hoax is to promote the drinking of bleach, which as I like to point out will successfully kill the virus, but unfortunately at the cost of killing the patient as well). This past week — April 24 or so — Donald Trump mused aloud at a press conference that maybe injecting disinfectants might work. In the days that followed, hundreds of people called 911 after swallowing cleaning fluid of various kinds, but Trump said he wasn’t to blame.
I went back and looked at some email newsletters I subscribe to that I hadn’t gotten around to reading from the end of February, and none of them even mentioned the coronavirus (which was still concentrated in China, and seen as not a big threat elsewhere). It was refreshing to read them, since everything is pretty much all COVID-19 all the time now, but it also felt surreal. Those newsletters were from less than a month ago, but it felt like they were from 10 or even a hundred years ago. When I started writing this post around March 19 or so, Italy (which only had 200 cases and no deaths at the end of February) had more than 20,000 cases. As of March 27, it had more than 86,000 cases and more than 900 deaths in a single day. Bodies were piling up in churches.
(Update March 29: Italy now has more than 97,600 cases and over 10,700 people have died, with more than 800 on March 28th alone. Update April 2: Italy now has 115,000 cases and almost 14,000 deaths but the curve appears to be flattening. Update April 9: 139,000 cases and 17,669 deaths — including almost 100 doctors and about 25 nurses. Update April 29: 200,000 cases and 27,000 dead, but only 200 or so died on April 24, the lowest death rate since March 14. Update May 9: total cases at 219,070 and deaths at 30,560 but rate of new cases and deaths are both falling).
-When we left for our vacation in Florida on March 7, we were aware that something bad was floating around, and made sure to wash our hands etc., but thought nothing of going to the beach or the pool and going out to restaurants. About 10 days later, we were anxious to get home because the rate of infection and death was climbing in the US — in part because of a lack of testing, caused by delays and screw-ups by the CDC and the Trump administration — and businesses (including airlines) were shutting down. The day after we got back, on March 19th, Canada and the US announced they would be closing the border to everything except goods, and the US closed its airports to traffic from Europe.
Update April 9: So far Canada doesn’t have a huge number of cases — 19,277 and 435 deaths — but there are hotspots such as a senior’s home in Bobcaygeon where 28 people have died). On March 24th, the Italian government put the entire country on lockdown, with fines for those who leave their homes without permission. As of March 26, the country’s police forces had charged more than 100,000 people with breaching the quarantine rules, which carries a fine of up to 3,000 Euros. Update April 9: In the UK, phone and email tip lines were swamped with reports of people breaching the rules and police were handing out fines.

In the US, state responses are still all over the map. As of March 25th, some states including Florida were still refusing to impose a state-wide lockdown (Update: Florida finally started shutting down parks and beaches at the end of March and then started reopening them April 18). As of March 27 Florida, Texas, and Rhode Island were all stopping people with New York and in some cases Louisiana plates and adding them to a state registry, and warning them to isolate themselves for at least 14 days or face civil penalties (Trump said March 28th that he was considering a quarantine for New York, New Jersey, and parts of Connecticut, but later said it was not necessary). A colleague of our next-door neighbour’s, who crossed the border from the US into Canada around March 25th or so, says he was told by the Canadian border guards that his license plate would go into a database, and if his car was seen anywhere other than in his driveway he could be fined up to $1 million and jailed for three years under the Quarantine Act.
Over the past couple of weeks (this was written May 8), there has been increasing pressure in a number of states from those who want restrictions on businesses and social activity loosened. There have been dozens of demonstrations in different states, many of them apparently organized by right-wing groups, including some that would only happen in the US: groups of men in camouflage with assault weapons in the gallery in the state capitol in Michigan, men with rocket launchers and anti-aircraft weapons in a Subway, and so on. A security guard was shot, apparently for refusing someone entry to a Family Dollar store because their child didn’t have a mask, and two employees at a McDonald’s were shot after telling someone that the fast-food restaurant was closed due to the coronavirus.
Since I started writing this post, the US has gone from fewer than 20,000 cases to more than 100,000 (making it the country with the largest number of infections, and that number continues to double roughly every 3-4 days (Update March 29: 133,000 cases and 2,300 dead Update April 2: 245,000 cases and 5,800 dead Update April 6: 360,000 cases and 10,700 dead Update April 9: 437,000 cases and 15,000 dead. Update April 28: Over 1 million cases and 59,000 dead — more than the Vietnam War. Update May 9: the US now has 1.3 million cases and 75,000 deaths, which means with just five percent of the world’s population, the US has nearly 33 percent of the infected and close to the highest number of deaths as well).
New York became the newest global hotspot at the end of March, with infections doubling roughly every two days. Hospitals there were quickly overloaded — New York state ordered 85 freezer trucks on March 26th to use emergency storage for bodies until they could be buried or burned, and bodies started piling up in morgues. Some models say even if self-isolation rules are maintained, the US could be looking at more than 120,000 dead before the current phase of the virus runs its course in August (Update: As of June 26th the US had already passed this number).
Some nurses and doctors in New York were wearing garbage bags because they ran out of protective clothing. Fashion manufacturers started making masks and hockey equipment companies began turning out face shields. On March 24, New York emergency services got more medical 911 calls than they got on September 11, 2001. (Update April 6: The chair of New York city council’s health committee said that all the 80+ freezer trucks are full of bodies — each truck holds 100 bodies — and so they might have to start burying people in parks or on Hart Island, where more than a million people whose bodies weren’t claimed are buried in a “potter’s field.” Trench graves are dug by prisoners from Riker’s Island). New York started burying on Hart Island in early April.
After returning to our home near Peterborough, just north of Toronto, on March 17 we tried to remain isolated for the 14-day quarantine, even from our neighbours (our houses are separate, but joined by a common atrium area). We used gloves to open doors in the common area, and stayed at least six feet from them even when we were outside. The only real issue was whether we needed to be careful about petting their dogs, which move back and forth between our houses. From what I could tell, pet fur isn’t a particularly hospitable place for viruses to live, and some epidemiologists say not to worry about petting your dog or cat, but it is impossible to know for sure (Update April 9: There are reports that cats can contract COVID-19, and a tiger at the Bronx Zoo reportedly tested positive).
The virus lives for quite a long time in the air after someone sneezes or coughs, and can live for hours or even days on surfaces like cardboard and stainless steel (however, this critical-care doctor at Cornell Medical Center in New York says in this video posted March 27 it appears that the vast majority of cases come from sustained physical contact with an infected person, and the CDC says infection from surfaces is possible, but not the primary way the virus is transmitted). A number of studies of hotspots in China and elsewhere showed that even within an enclosed space like a restaurant, the main risk was to people who were downwind of the infected person or within the radius of air blown from the indoor air-conditioning unit.I am almost 60 and have asthma, but we feel as though our risk is fairly small (despite having flown through two airports to get back to Canada).
As I write this on March 27 we are on day 10 of our quarantine (Update April 9: We came out of quarantine on April 1 but are still isolating — only one of us goes out for groceries every few days. We did have two friends come to stay in the old farmhouse nearby, which we thought would be okay because we stayed away from them for the most part. But we did eat together (on opposite sides of a ten-foot-wide table) which made our daughter and son-in-law — both nurses — quite upset. In our defence, we were trying to help our friends stop going stir crazy and thought we took enough precautions, but we may have been wrong about that. Let’s hope we don’t wind up paying for it. Update April 28: We now have a friend staying in the old farmhouse who came back to Canada from Spain, but we only see her when she comes outside for walks.
A woman I work with said in March that she and her husband and 11-year-old daughter — who has severe asthma — all had what appears to be COVID-19, but they couldn’t get tested because they don’t meet the criteria. As of March 27 they were on day 21 of their self-quarantine and still had a fever and shortness of breath (Update April 9: They seem to be improving, but are still not at 100-percent health). Her doctor wanted her to start using an anti-malaria drug that has shown promise in some tests (hydroxychloroquine) but she can’t get approval unless she is confirmed to have the virus — and a number of doctors are warning against use of a drug that hasn’t been properly tested. The French doctor whose study showed it might have promise is known for publishing manipulated data, and his study was not scientifically approved or controlled. Hydroxychloroquine can also have some fairly severe side effects involving the eyes and other parts of the body. (Update April 9: Some hospitals have stopped their tests of the drug because of side effects, in some cases death, but there are still many promoting it as the closest thing to a cure. Some doctors who have tried it say it doesn’t really help).
Even after the virus started killing large numbers of people, some people — including the president of the United States — argued that it wasn’t that different from the seasonal flu, which kills about 400,000 people every year, mostly those who have underlying conditions or compromised immune systems. Some said it was a lot of noise over nothing, like the H1N1 was (a line of argument that shows up in the movie Contagion). But experts quickly countered this with facts. Yes, we lived through SARS in the early 2000s (which was also a form of coronavirus) and then H1N1 in 2009, but while they seemed pretty bad, they weren’t even close to what we are up against with COVID-19. Both SARS and the most recent version of H1N1 (also called “swine flu”) were significantly less dangerous than the current virus is, in part because they were so lethal.
In other words, they killed people really quickly, which means from a viral point of view they weren’t very successful, because they didn’t spread as quickly or as widely as they might have. The fatality rate for SARS was in the 10 percent range, while COVID-19 appears to only kill about 2-4 percent of those infected (of course, if billions are infected, that’s still a large number). Experts say that mortality rate may come down to 1 percent or lower as there is more testing — but also point out that death rates are also likely being under-counted by a significant amount. According to recent research, a significant number of people who get COVID-19 are infectious even when they don’t have symptoms, so it’s impossible to know whether they have the virus or not, because most don’t get tested (except in countries where they are doing random testing, like South Korea — which seems to have been the most effective at halting the spread). And so they go about their lives normally, contacting other people and infecting them without realizing it. Also, according to this epidemiologist, there are signs that people can remain infectious for up to three weeks even after they recover and show no symptoms.
tThe the so-called “R nought” for COVID-19 — the number of people who are infected by anyone carrying the virus — is estimated to be much higher than other similar viruses. For swine flu it was about 1.5, and for COVID-19 it is estimated to be as high as 2.5 (although that changes based on the number of people tested, and could wind up being lower). So by the time a country or region figures out that people are dying from COVID-19, there are likely thousands of un-diagnosed cases wandering around or thinking they only have the regular flu. According to figures compiled by Thomas Pueyo — in a persuasive Medium piece about why countries needed to shut down completely and quarantine as many people as possible — at this point in the region of China where COVID-19 started, for every death that was recorded, approximately 800 people were already infected. The US has about 75,000 deaths as I write this (updated May 9), which suggests it may have more than 60 million infected people — a study in Iceland showed that as many as 50 percent of people don’t show any symptoms.
Unfortunately, Pueyo points out that while China and South Korea both shut things down relatively quickly and were able to escape the worst of the exponential increase in infections, the US delayed and delayed before shutting down incoming flights, large gatherings, etc. And that could mean by the time the US figures out how many cases it has, it could be too late to stop the health-care system from becoming overloaded, leading to even more deaths. Pueyo’s model projects a worst-case scenario of deaths rising to 10 million — a number that is much higher than an Imperial College study, mostly because he is including collateral effects: in other words, hospitals won’t have enough beds, respirators and doctors to treat all the people who need it — not just coronavirus patients, but anyone with a serious illness — and so large numbers of those people will die who otherwise wouldn’t have. In Italy, hospitals are turning away people who are over 70 because there is no point in treating them, and the resources are needed for others.

There have been a number of other articles (although notably, none by epidemiologists or even doctors) arguing that the US has gone overboard in shutting down businesses, closing schools, etc. because this is going to wreck the economy. According to this argument, since the coronavirus mostly attacks old people and those with underlying health problems, we should spend most of our time isolating those people, but allow others to go to school and work normally (there’s a thread from a biologist debunking much of the Medium piece linked above, which Medium took down, at which point it was republished at Zerohedge, a site known for its right-wing conspiracy theories). Experts at the CDC and elsewhere, however, say this approach — which the British government considered implementing, in the hope that “herd immunity” would develop — would result in an unacceptable number of acute cases, which would cripple the medical system. This report from the Imperial College of London helped change the mind of British legislators (on March 27th, UK prime minister Boris Johnson said that he had tested positive for the virus — Update: on April 5th he was admitted to hospital and on April 6th he was moved to intensive care, but he responded to treatment and was later released). During the week of May 9, it was reported that multiple people have tested positive for the virus in the White House, including one of the personal valets to Donald Trump, as well as another senior aide.
As a thread from a scientist on Twitter points out, the numbers we are seeing right now are the result of decisions that were made as long as three weeks ago. Interestingly enough, Sweden appears to be taking the same approach that Britain did initially — it is the only country in Europe that hasn’t implemented some kind of restriction on the movement of citizens. The country has asked people not to gather in groups of more than 50, but compliance is voluntary — one article about the Swedish decision pointed out that it relies on the trusting nature of its citizens, but another noted that as of April 28, the country’s death rate was 22 per 100,000 or about three times as high as its neighbour Denmark. Which raises the question: Is that an acceptable level of deaths? Only Sweden can really answer that question.
Since China was the first place COVID-19 was spotted, everyone is watching what is happening there, especially since the country appears to have been successful in clamping down on the populace in the Hubei region to the point where it hasn’t had a domestically produced case of the virus for three days. The big question is what happens when China eases the restrictions that got it there — will new cases start to appear, as they already have? If those who have the virus are still infectious for three weeks after they have recovered, what does that mean for the numbers of new infected patients in China? Pueyo argues that authorities will have to ease restrictions and then watch the R nought value, and then reimpose restrictions when it rises too far, and keep doing that potentially for months or even a year, until a reliable vaccine is developed. Meanwhile, there is a lot of emphasis on “contact tracing,” to track who has been exposed. Experts say the US would need as many as 300,000 people working as contact tracers, but there were only 8,000 as of May 9. Google and Apple are said to be collaborating on an update to their operating systems that would allow people to be notified if they were in contact with someone who later tested positive, but some say there are flaws with that system. “To me, it’s just techies doing techie things because they don’t know what else to do,” said security expert Bruce Schneier.
(Update March 27: There have also been questions raised about the true level of deaths in Wuhan, as cremation urns turn up by the thousands in front of funeral homes in that region. Update April 1: A US intelligence report suggests they are almost certainly fudging the numbers for both infected and deaths, and sources agree many people dying of COVID-19 in the US aren’t being counted either). Also, there are questions being raised about whether the presence of antibodies after fighting off the disease means that someone is immune — and the WHO is saying there is not enough evidence to make that case. On an unrelated note, some doctors say they are seeing a lot of COVID-19 patients, including those in their 20s and 30s, die of sudden strokes or aneurysms, because the virus appears to cause a strange form of clotting problem. And even after this many deaths, doctors say they aren’t even sure exactly how it kills people exactly — it seems to have effects on almost every organ. It also appears to have lasting effects on the body even after people recover.
This is all pretty anxiety-inducing, the reality of what this virus means, especially for friends who are immune-compromised because of cancer, or have lung issues, or those in the health-care field (like our eldest daughter and her husband, who work in intensive care and emergency medicine). But it’s important to remember that there are still plenty of bright spots, as I remind myself every time I go for a walk in the woods with the dogs and see the birds and the new lambs in the field near our house (here’s a recent photo). There are also groups of people banding together to help the less fortunate, to go shopping for the elderly or quarantined, and engineers using 3D printers to make medical equipment. Museums are streaming their collections for free, orchestras are putting on concerts online, etc. And then there’s rugby commentator Nick Heath, who has no sports to cover any more, so he has taken to doing color commentary on everyday life. Stay safe, everyone! Somehow we will get through this together.
